Article seen originally in Chemistry World
In labs at Imperial College London, UK, researchers are studying how tiny groups of neurons and other cells only just visible to the naked eye respond to antidepressants. Parastoo Hashemi’s team hopes that these ‘mini-brain’ organoids will finally help us understand how drugs such as selective serotonin reuptake inhibitors (SSRIs) work in full-sized brains.
2024 marks 50 years since researchers published the first paper on the first SSRI, fluoxetine, which came to market as Prozac in 1988. Today, SSRIs are widely used to treat depression: in England in 2022, 46 million prescriptions for SSRIs were dispensed, with 21 million of those for the SSRI sertraline, making it the 10th most prescribed drug that year. That compares to 57 million prescriptions for the most prescribed drug, atorvastatin, in the same year.
As such it might seem strange that researchers like Hashemi still don’t fully understand how SSRIs work, and why they work better for some patients than others. In fact, researchers have struggled to balance the drugs’ benefits with their shortcomings for decades. In 2004, Chemistry World reported findings that they only work slightly better than taking an inactive placebo. At the same time, concerns around increased risk of suicide among patients, especially children, taking SSRIs came to prominence. SSRIs also have other potentially serious side effects.
Experiments involving mice have suggested that some signaling molecules mark depression and relate to how well antidepressant drugs, specifically SSRIs, work. Hashemi’s mini-brain experiments are therefore focused on monitoring levels of these molecules, including the inflammation mediator histamine and the mood-affecting neurotransmitter serotonin.
Hashemi’s group makes organoids from a person’s own cells. The scientists then integrate them with chips that monitor how tiny electrical currents in the cells change as the researchers wash the organoids with a solution of a drug. The fluctuations relate to the levels of histamine and serotonin. ‘We think those chemical signals can give an indication of whether the drug is going to be effective,’ Hashemi tells Chemistry World. She hopes that her team’s measurements will help identify differences between people, showing ‘which drugs they’re going to respond to, which combinations, which doses’.
Despite the gaps in our knowledge of SSRIs, the drugs still have an important role, comments Eero Castrén from the University of Helsinki, Finland. ‘It is certainly true that that there is much to be improved in the effectiveness of antidepressants,’ he says. ‘But it’s also widely accepted that they do work on many patients. Not all the patients, not all the time, not all the conditions. But for many, many patients, they do have an effect.’
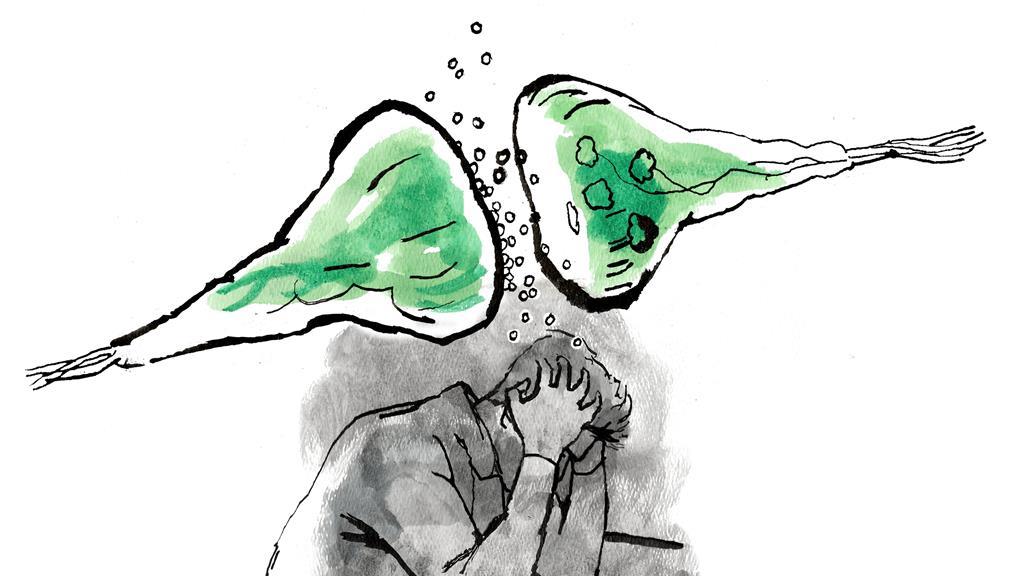
SSRIs remain controversial, however, as biochemical and social views on depression collide. Biochemical researchers want to know what is happening in our brains during depression, and whether we can use those processes to help sufferers. Social researchers, meanwhile, point out that drugs only treat the symptoms of depression, which can mask or distract from the more fundamental issue of addressing its societal causes . The uncertainty over how SSRIs work is a key area for conflict. But why does that uncertainty persist?
Fixing the wrong problem?
One reason for uncertainty is that SSRIs came soon after drugs sold in the 1950s that boosted patients’ moods accidentally. One of those was the tuberculosis drug iprionazid, which researchers found stopped the enzyme monoamine oxidase breaking down the neurotransmitters noradrenaline, serotonin and dopamine. ‘It made [patients] happier,’ says Hashemi.
Imipramine, invented as an antihistamine allergy treatment, inadvertently became the first in the tricyclic antidepressant drug class. Scientists don’t understand exactly how these antidepressants work, but we know they interact with receptor proteins that help pass signals through the neuron cells in our brains. Tricyclics affect many such receptors, including those that send signals when noradrenaline, serotonin and dopamine bind with them. Neurons release these neurotransmitters into structures called synapses to bridge gaps with adjacent neurons, sending signals on to their neighbours.
In the 1960s, researchers looking to minimise side effects focused in on one specific protein: the serotonin transporter protein. This protein mops up serotonin molecules that neurons have released into the synapse gap and transports them back to where they came from. Drugs like fluoxetine are designed to block this reuptake process and raise serotonin levels in the synapse, giving SSRIs their name. But evidence has since shown that serotonin transporter blocking is likely not the most important action of the original lucky antidepressants finds.
For example, various studies have shown that serotonin levels don’t directly correlate with depression. In 1994, researchers stopped untreated depressed people eating tryptophan, the amino acid our body makes serotonin from. The patients’ depression didn’t rapidly worsen. For some, it did worsen, but more slowly than the scientists would have expected if serotonin was directly responsible. The difference between these patients may relate to why SSRIs work better for some people than others.
Castrén notes that such person-to-person variation is fairly normal in medicine. ‘There are lots of drugs for blood pressure, and they don’t work for many people,’ he says. ‘But nobody’s complaining about that.’ The stigma surrounding mood disorders makes antidepressants more controversial, Castrén says.
The SSRI controversy turned into widespread shock in 2022, thanks to a review paper by psychiatrist Joanna Moncrieff from University College London and colleagues. We’ve become so used to the idea that depression is linked to a serotonin imbalance that their conclusion there is no evidence for low serotonin levels causing depression stunned the world. ‘We’ve never known how [SSRIs] work,’ Moncrieff says. While they may raise serotonin levels in the short term, Moncrieff argues that this is changing our brain’s baseline chemistry. She compares the effect to that of drinking alcohol.
People link serotonin and depression more closely than they should, Moncrieff emphasises, and has a suggestion for why. ‘There’s a strong desire among the medical profession to see depression as a biological condition, and to believe that we have a treatment that will help,’ she says. ‘People have come to expect and to want a chemical treatment for their low mood.’
Moncrieff argues that drug companies, doctors and psychiatrists benefit from this situation because it’s profitable. She also suggests that it’s convenient for policy makers to support their use to avoid tackling ‘endemic social discontent’ in other ways. So, perhaps what Moncrieff calls the antidepressants’ ‘perceived usefulness’ has prevented us from more thoroughly questioning how they work.
‘If you’re a politician, you can just move it over to the experts, rather than having to think “Why are so many people in our society unhappy?”’ she says. ‘Could it be to do with financial insecurity and poverty and inequality? We are medicalising the consequences of social and economic policies that render some people inactive, unemployed and insecure in housing and finances.’
Growth area
Hashemi focuses on depression’s biochemical basis. ‘If you experience something that causes stress, it permanently then changes your brain structure and chemistry,’ she says. ‘Moving forward, you change your behaviour. The chemicals determine how you change your behaviour.’
Many people have taken Moncrieff’s 2022 paper as a reason to attack SSRIs and psychiatry in general, Hashemi notes. ‘We know [SSRIs are] not perfect,’ she says. ‘Nobody loves them. But they work, and they work quite well for a subset of patients. The public is becoming susceptible to quite dangerous anti-SSRI rhetoric that can really be harmful to the people who need them. I think we have to be really clear that that’s not based on science.’
Yet Hashemi accepts that not fully understanding the chemical and physiological reasons makes it difficult to explain some SSRI quirks, like the differences between individuals. However, she notes that some people who don’t respond to SSRIs have a specific version, or polymorphism, of the gene carrying instructions for how to make the serotonin transporter protein. This is one topic her team is intending to study with its mini-brains.
While Castrén notes that most patients don’t care exactly how SSRIs work, his team has helped find a promising new potential explanation. The scientists have focused on the role of Brain Derived Neurotrophic Factor (BDNF) protein. BDNF helps keep neurons alive as well as enabling plasticity, the process in which neurons grow and change their connections. In the 1990s, researchers found that in tests on animals that simulate depression reduced BDNF secretion leads to fewer synapses. Injecting BDNF straight into their brains could increase the number of synapses, and reverse depression-like behaviour.
In the early 2000s researchers found SSRIs promote neurons to grow in brain areas such as the prefrontal cortex, Castrén highlights. ‘We thought that this is an indirect effect of the actual serotonin,’ he says. In recent years, Castrén’s team has found that antidepressants bind directly with the receptor protein on neurons that recognises BDNF, called TrkB. ‘For plasticity, and in mice for antidepressant-like behavioural responses, binding to TrkB seems to be necessary,’ Castrén says. ‘In our mind, the critical things that antidepressants do is bind to TrkB.’
Castrén hopes that SSRI effects on plasticity might reconcile ideas about social and biochemical factors. A person’s social environment, potentially including psychotherapy, must help support better mental health while drugs trigger plasticity. ‘You need both,’ Castrén comments. However, he notes that SSRIs ‘are cheaper than candy’, whereas support in the form of psychotherapy is very expensive. ‘With the number of people suffering from depression, it’s hardly possible to even think about having a psychotherapist for all of these people.’
The recent focus on SSRIs has driven research funding in the area, says Hashemi, ‘because there’s a huge need for it’. She thinks this could lead to important advances, especially in using pre-clinical screening and AI to develop better antidepressants. ‘We’ve got five to ten years of interesting developments ahead of us,’ she says.
Ultimately, Hashemi is confident that scientists can solve the SSRI puzzle, citing the 80 years it took to work out how aspirin worked. ‘People have lost patience with the process with SSRIs,’ she says. ‘But that doesn’t mean the community is not working full time trying to understand how they work. We don’t have the technology that we need right now. But we will, it’s just a question of time.’